Offering targeted support to group plan members with high-cost chronic conditions is the key to protecting benefit sustainability, says the Express Scripts Canada Prescription Drug Trend Report: Trends in Canadian Private Benefit Plans released last week.
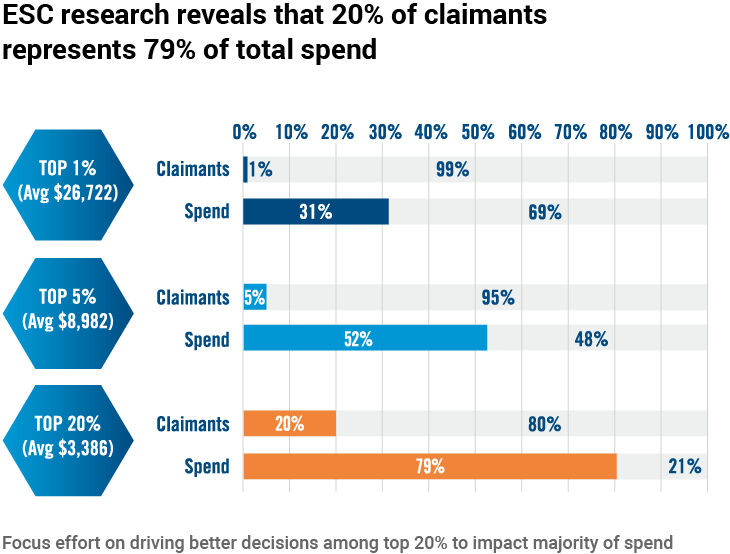
Representing 20 per cent of claimants, members with high-cost chronic conditions drive almost 80 per cent of plan costs with an average annual drug spending that is 15 times that of other claimants, says the report.
Source: Express Scripts Canada Prescription Drug Trend Report, 2018
Specialty drugs
Private plan spending on prescription drugs rose by 2.5 per cent from 2016 to 2017, according to Express Scripts Canada’s findings. Spending on specialty drugs continued to increase with these drugs now accounting for 31 per cent of the total prescription plan spend – up from 15 per cent in 2008.
“This trend shows no signs of slowing down, with specialty drugs representing a majority of new drugs in the development and approval stages,” says the report.
Members with high-cost chronic conditions “have, on average, 7.8 chronic conditions, see 3.3 physicians and take 8.9 medications – understandably, they struggle with the complexity of their treatments.”
Gaps in adherence
About half of these members are non-adherent to one or more of their medications and gaps in adherence “can possibly lead to worse health outcomes, and ultimately even greater costs for the drug plan,” warns the report.
“Year after year, we see increases in the amount spent by prescription drug plans,” said Express Scripts Canada president Mike Biskey. “And the majority of these costs are concentrated on a relatively small number of claimants. Clearly, there is an opportunity for better health and financial outcomes if we actively engage and guide this group, and we can do that through comprehensively managed plans.”
To learn more, read the full report on the Express Scripts website.




